- Stock: In Stock
- Brand: Acme Laboratories Limited
- Product ID: Levothyroxine Sodium
100% Secure Payment

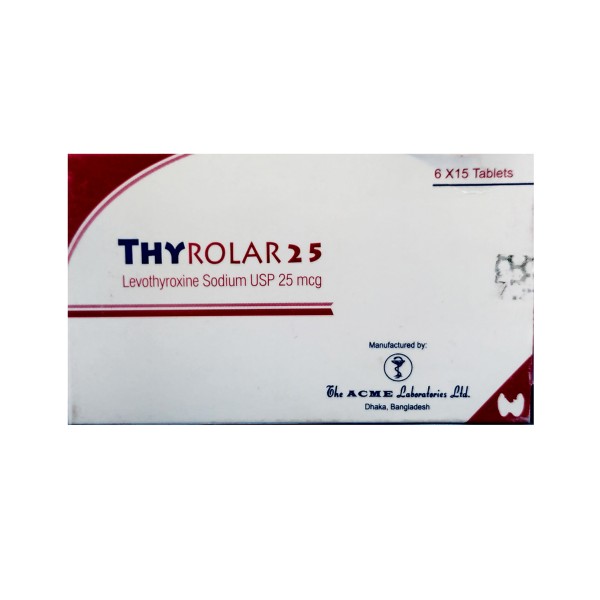
Thyrolar 25 mcg Tablet
DESCRIPTION
Levothyroxine is a synthetic thyroid hormone, identical to thyroxine (T4) that is produced and released by the thyroid gland. In the peripheral tissues, T4 is converted to T3, the active metabolite, by deiodination. T3 and T4 diffuses into the cell nucleus and bind to the thyroid receptors attached to
DNA. This activates gene transcription and synthesis of mRNA and cytoplasmic proteins. Thus thyroid hormones regulate multiple metabolic processes and play an essential role in normal growth and development, and maturation of CNS and bone. Levothyroxine is effective as replacement or supplemental therapy in natural thyroxine deficiency.
COMPOSITION
Thyrolar 50 mcg Tablet: Each tablet contains Levothyroxine Sodium USP 50 mcg.
INDICATION
Hypothyroidism: As replacement or supplemental therapy in congenital or acquired hypothyroidism of any etiology, except transient hypothyroidism during the recovery phase of subacute thyroiditis.
Specific indications: Primary (thyroidal), secondary (pituitary), and tertiary (hypothalamic) hypothyroidism and subclinical hypothyroidism.
Pituitary TSH Suppression: In the treatment or prevention of various types of euthyroid goiters, including thyroid nodules, subacute or chronic
lymphocytic thyroiditis (Hashimoto's thyroiditis), multinodular goiter and, as an adjunct to surgery and radioiodine therapy in the management of thyrotropin-dependent well-differentiated thyroid cancer.
DOSAGE AND ADMINISTRATION
The goal of replacement therapy is to achieve and maintain a clinical and biochemical euthyroid state. The goal of suppressive therapy is to inhibit growth and/or function of abnormal thyroid tissue. Dosing must be individualized and adjustments made based on periodic assessment of the patient's clinical response and laboratory parameters.
Thyrolar is administrated as a single daily dose at a fixed time preferably one-half to one hour before Breakfast. Thyrolar should be taken at least 4 hours apart from drugs that are known to interfere with its absorption.
Thyrolar may be administered to infants and children who cannot swallow intact tablets by crushing the tablet and suspending the freshly crushed tablet in a small amount (5-10 ml or 1-2 teaspoons) of water. This
suspension can be administered by spoon or dropper. Do not store the suspension.
Adult Dosage
In hypothyroidism the initial adult dose is 50-100 mcg once daily, with gradual increments of 25-50 mcg at about 4 weeks intervals until the thyroid deficiency is corrected and a maintenance dose (Usually100-200 mcg/day) is established.
In elderly patients in those with cardiovascular disorders, or in those with severe hypothyroidism of long standing, treatment should be started more gradually: Initial dose is 12.5 to 25 mcg/day increased by increments of 12.5 to 25 mcg at intervals of about 4 weeks.
Pediatric Dosage
Levothyroxine therapy of children should be instituted at full replacement doses as soon as possible, with the recommended dose per body weight decreasing with age. mcg/day of levothyroxine sodium is recommended with increments of 25 mcg every 2-4 weeks until the desired effect is achieved. In infants with very
low (< 5 mcg/dL) or undetectable serum T4 concentrations, the recommended initial starting dose is 50 mcg/day. A lower starting dose (e.g. 25 mcg/day) should be considered in infants at risk for cardiac failure. The dose should be adjusted based on clinical response and laboratory parameters.
Hyperactivity in an older child can be minimized if the starting dose is onefourth of the recommended full replacement dose, and the dose is then increased on a weekly basis by an amount equal to one-fourth the fullrecommended replacement dose until the full recommended replacement dose is reached.
OR AS DIRECTED BY THE PHYSICIAN.
SIDE EFFECTS
Adverse reactions associated with levothyroxine therapy are primarily those of hyperthyroidism due to therapeutic overdosage. They include the following:
General: fatigue, increased appetite, weight loss, heat intolerance, fever, excessive sweating;
Central nervous system: headache, hyperactivity, nervousness, anxiety, irritability, emotional lability, insomnia;
Musculoskeletal: tremors, muscle weakness;
Cardiac: palpitations, tachycardia, arrhythmias, increased pulse and blood pressure, heart failure, angina, myocardial infarction, cardiac arrest;
Pulmonary: dyspnea;
GI: diarrhea, vomiting, abdominal cramps;
Dermatologic: hair loss, flushing;
Reproductive: menstrual irregularities.
CONTRAINDICATION
Levothyroxine is contraindicated in patients with untreated subclinical or overt thyrotoxicosis of any etiology and in patients with acute myocardial infarction or with known hypersensitivity to any ingredient of it.
PRECAUTION
Careful dosage titration is necessary to avoid the consequences of over- or under-treatment. Caution is needed in patients with cardiovascular disorder, diabetes mellitus or diabetes insipidus, nontoxic diffuse goiter or nodular thyroid disease and to the elderly one.
PREGNANCY AND LACTATION
Pregnancy - Category A and may increase levothyroxine requirements.
Nursing mother: Although thyroid hormones are excreted only minimally in human milk and usually safe in nursing mothers, caution should be exercised when it is administered.
DRUG INTERACTION
Thyroid hormones enhance the effect of oral anticoagulants. Patients on anticoagulant therapy therefore require careful monitoring when treatment with thyroid drug is started or altered as the oral anticoagulant dose may need to be adjusted. In hypothyroid diabetics, starting thyroid replacement therapy may increase their insulin or oral hypoglycemic requirements. So careful monitoring of diabetic control is recommended, especially when thyroid therapy is started, changed, or discontinued. Intravenous administration of epinephrine to patients with coronary artery disease may lead to complications ranging from difficulty in breathing to a heart attack and therefore careful observation is needed. Concurrent use of antacids, sucralfate, and calcium carbonate may reduce the efficacy of levothyroxine by binding and delaying or preventing absorption. Levothyroxine should be taken at least 4 hours apart from these agents. Concurrent use of tri/tetracyclic antidepressants and levothyroxine may increase the therapeutic and toxic effects of both drugs, possibly due to increased receptor sensitivity to catecholamines. Toxic effects may include increased risk of cardiac arrhythmias and CNS stimulation; onset of action of tricyclics may be accelerated. Converting hypothyroidism to the euthyroid state with
levothyroxine may increase the blood level of theophylline and it may be necessary to change the dose of theophylline. Administration of sertraline in patients stabilized on levothyroxine may result in increased levothyroxine requirements. Levothyroxine therapy may decrease the actions of certain beta-blocking drugs and therefore to change the dose of beta-blocker. For the same reason, the dose of Digoxin also may need to be changed.
OVERDOSE
Excessive dosage results in a hypermetabolic state. The signs and
symptoms of overdosage are those of hyperthyroidism. In addition, confusion and disorientation, cerebral embolism, shock, coma, and death may occur. Symptoms may not necessarily be evident or may not appear until several days after ingestion of levothyroxine sodium.
Levothyroxine sodium should be reduced in dose or temporarily discontinued if signs or symptoms of overdosage occur.






























